Status Epilepticus
1. Definition
Conventional definition: >30 min of
continuous seizure or convulsions or of intermittent seizures
without full recovery.
There is evidence that seizures of 30 minutes or longer
duration cause neuronal damage, and this is the basis for the
definition. However, do not wait for brain damage to
occur--treat for status epilepticus if the seizure has lasted
more than 5 to 10 minutes.
2. Classification of status
- Generalized
-
- Convulsive
- Nonconvulsive
-
- Absence
- Late stage of convulsive
- Partial
-
Generalized motor status is a true medical emergency
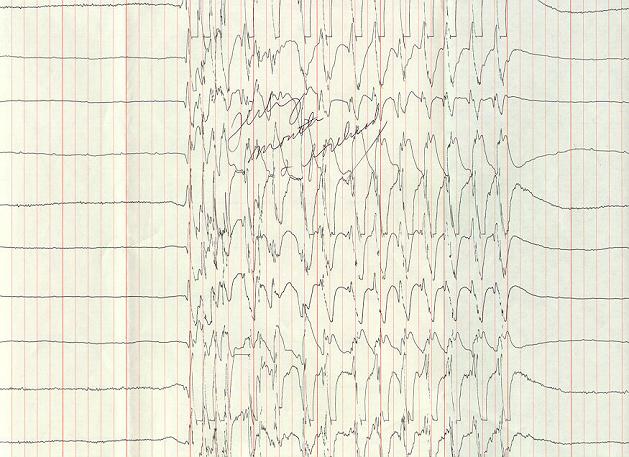
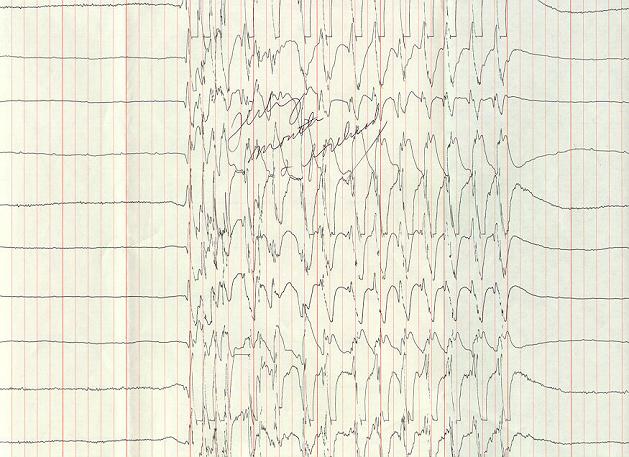
3. Stages of status epilepticus
- Discrete seizures
- Merging seizures
- Continuous ictal activity
- Continuous ictal activity, punctuated by low voltage
flat activity
- Periodic epileptiform discharges on a quiet
background
(Treiman et al. 1990)
4. Systemic complications of status
- Lactic acidosis
- Hypo- or hyperglycemia
- Hyperpyrexia
- Dehydration
- Shock
- Rhabdomyolysis
- Death
5. Mortality of status epilepticus
- Dead of status 1.8%
- Dead of underlying cause 28.8%
- Dead other causes 6.5%
- Alive 63.1%
6. Mortality of status epilepticus
|
A comparison of survival by duration in status
epilepticus shows a marked increase in mortiality
for patients in prolonged status epilepticus.
(Towne et al. 1994)
|
 |
7. Neuronal death
- Cerebral cortex (laminar necrosis)
- Hippocampus
- Amygdala
- Thalamus
- Cerebellum
8. Epilepsy
- Status epilepticus can produce epilepsy.
- 20 to 40% of persons develop epilepsy after an episode
of status epilepticus. (Hesdorffer et al. 1998)
- The mechanism of this could be damage to
hippocampus.
9. Important!!
Eliminate the electrical seizure to
prevent neuronal injury in status epilepticus
10. Steps in treatment
- ABC's
- Quick assessment
- Stop the seizure
- Find the cause
11. Quick assessment
History:
|
seizures?
stroke?
head trauma?
neoplasm?
medical noncompliance?
alcohol or barbiturate use?
theophylline use? |
Examination:
|
fever?
papilledema?
elevated blood pressure?
focal seizure onset?
focal neurologic exam? |
12. Causes of status
Medication withdrawal
CVA
Alcohol withdrawal
Idiopathic
Anoxia
Metabolic disorder
Hemorrhage
Infection
Tumor
Trauma
Drugs
CNS infection
Congenital brain injury |
22.5%
22.5%
14.2%
14.2%
11.9%
11.5%
5.1%
5.1%
4.4%
4.0%
2.4%
0.8%
0.8% |
Some patients have more than one etiology.
(Towne et al. 1994)
13. Laboratory studies often useful
- Blood glucose, sodium, calcium, magnesium, creatinine,
BUN, ABG, anticonvulsant levels
- CBC, CPK, toxicology screen
- CT scan w/o contrast
- Lumbar puncture
- EEG
14. Simple procedures always recommended
- Pulse oximetry
- Continuous ECG
- IV
15. Initial Rx for seizures
If hypoglycemic, then:
- IV glucose (50 cc D50)
- Thiamine (10 mg IV + 90 mg IM)
16. Anticonvulsants
- Standard:
-
Lorazepam
Diazepam
Fosphenytoin
Phenytoin
Phenobarbital
- Useful:
-
Valproate
Midazolam
17. Benzodiazepines
- Use a benzodiazepine first. They work quickly, and
status epilepticus is more difficult to control if
treatment is delayed.
- Lorazepam 4 - 8 mg (0.1 mg/kg) IV
-
- Slower onset, longer duration
- Diazepam 5 - 20 mg (0.15 - 0.25 mg/kg) IV
-
- Rapid onset, short duration
- Give IV push
- Be prepared to intubate
- IV diazepam is not useful for serial
seizures
18. Diazepam has a short duration of action
|
Diazepam has only a short duration of action. This
is primarily because it quickly redistributes from
brain to fat. Note that plasma diazepam
concentration is less than half its peak ten
minutes after an IV infusion.
(Ramsay et al. 1979)
|
 |
19. Phenytoin
- Loading dose 18 - 20 mg/kg IV (1000 - 2000 mg)
- Rate < 50 mg/min. to avoid hypotension,
arrhythmias
- Never give IM
- Never in dextrose
- Loading dose works up to 18 hours
- Stops 80% of generalized motor status epilepticus
20. Fosphenytoin
- Prodrug of phenytoin for parenteral
administration
- Rapidly and completely converted to
phenytoin by nonspecific tissue
phosphatases
- Water soluble, pH 8.6 - 9
- Can be given IM
- No sterile necrosis or tissue
abscesses
- Molecular weight 1.5 times that of
phenytoin
|
 |
21. IV loading of fosphenytoin
 |
| Fosphenytoin is rapidly converted to phenytoin.
Plasma concentrations of phenytoin are essentially
identical whether phenytoin or fosphenytoin is
infused. |
22. Phenobarbital
- Loading dose 20 mg/kg IV
- Not > 100 mg/min
- Patient should be intubated
23. Intravenous valproic acid
- Depacon®
- Give an IV loading dose followed by a three times daily
dose of valproic acid by mouth or IV.
- Package insert says not faster than 50 mg/min (but I
have given it up to 200 mg/min, and this is probably
safe).
24. Serial seizures
- Fosphenytoin IV or IM
- Phenytoin PO
- Lorazepam IV or PO
- Oral antiepileptic drugs
- Diazepam rectal gel
- Not IV diazepam
25. Refractory status: midazolam
- Give midazolam as a continuous infusion
- Use EEG monitoring if possible, titrate infusion to
eliminate electrographic seizures.
- 200 micrograms/kg as a slow IV bolus, followed by 0.75
to 10 micrograms/kg/min.
- In the most refractory cases more than 10
micrograms/kg/min may be needed.'
- Hypotension is uncommon but may occur.
26. Refractory status: pentobarbital
- Administer pentobarbital as a continuous infusion.
- 5 mg/kg load, then 1-3 mg/kg/hour
- Must use EEG monitoring; goal is to titrate drug
infusion to EEG burst suppression.
- Hypotension is common; fluids and pressors may be
needed.
27. EEG burst suppression
 |
| A quiet EEG background is frequently interrupted by
bursts of high voltage activity. The high voltage
activity often contains epileptiform spikes or
spike-wave discharges. |
28. Other types of status epilepticus
- Generalized nonconvulsive status epilepticus
-
- May be a late stage of convulsive status
epilepticus
- Signs may be subtle: subtle facial twitching,
nystagmus, ocular deviation
- Myoclonic status epilepticus
-
- May follow anoxic encephalopathy
- May be stimulus-sensitive
29. Controversies in status epilepticus
- Significance of certain EEG patterns:
-
- Periodic epileptiform discharges (PLEDs)
- Bi-PLEDs
- Periodic discharges
- Frequent triphasic waves
- Titrate IV antiepileptic with EEG to:
-
- Burst suppression
-
- Easy to see, but may go flat before
burst suppression
- Elimination of seizure
-
- Sometimes hard to recognize
30. Periodic discharges
 |
| This patient had right frontal periodic discharges
and encephalopathy. Treatment with fosphenytoin and
valproate improved the discharges, but the patient was
clinically unimproved. |
31. Time table for treatment of status
a. 0-10 min, do ABC's:
- O2 by nasal cannula. Intubate if
necessary.
- Establish IV access.
- Draw glucose, serum chemistries, CBC, toxicology
screen.
- Draw antiepileptic drug levels if patient known to be
treated.
- Thiamine (100 mg) then glucose (50 ml of 50%) if
hypoglycemia demonstrated or suspected.
b. 10-20 min, administer a benzodiazepine
drug:
Lorazepam (0.1 mg/kg at 2 mg/min IV) or
diazepam (0.2 mg/kg at 5 mg/min IV). Lorazepam is the
drug of choice. Both drugs act quickly, diazepam slightly
faster, but it redistributes to fat quickly, and its effective
duration of action may be only 5-10 min. With diazepam,
repeated doses are often necessary. If diazepam is used,
phenytoin (or fosphenytoin) should next be given to prevent
recurrence of seizures. The effective duration of action of
lorazepam is 8-10 hours, and is recommended for initial
treatment of status epilepticus.
c. 20-60 min, administer fosphenytoin or
phenytoin
Fosphenytoin is a water-soluble
phosphate pro-drug of phenytoin. It replaces IV phenytoin,
which is highly alkaline (pH 12) and dissolved in 40% propylene
glycol/10% ethanol. It can be dosed using "phenytoin
equivalents". (Its molecular weight is 1.5 times that of
phenytoin.) Can be used IM. Can be given at a rate of 150
mg/min IV. Hypotension and cardiac arrhythmias are less common
than with phenytoin.
Phenytoin In adults give 18 mg/kg no faster
than 50 mg/min IV. Monitor ECG and BP during infusion. Do not
use glucose-containing IV solution. Purge IV line with normal
saline before infusion. Do not give phenytoin IM because
it may cause sterile abscesses. Ensure adequate IV access
because local infiltration of phenytoin can cause skin
necrosis.
d. >60 min
- Administer additional doses of fosphenytoin or
phenytoin up to a maximum of 30 mg/kg.
- Administer phenobarbital (20 mg/kg at 100 mg/min IV).
Assisted ventilation will usually be required.
e. If seizures persist:
- Pentobarbital infusion. 5 mg/kg load, then 1-3
mg/kg/hr. Must use EEG monitoring, goal is to titrate to
EEG burst-suppression. Avoid hypotension if possible, but
fluids and pressors may be needed.
- Midazolam drip. Use with EEG monitoring if possible,
titrate infusion to eliminate electrographic seizures. 200
micrograms/kg as a slow IV bolus, followed by 0.75 to 10
micrograms/kg/min continuous infusion. In the most
refractory cases more than 10 micrograms/kg/min may be
needed. Hypotension is uncommon but may occur.
- Propofol drip. Few advantages over pentobarbital.
- General anesthesia (isoflurane, ketamine).
- Paraldehye: no longer available.
- Diazepam drip. Used infrequently.
- Lidocaine drip. Used infrequently. May exacerbate
seizures.
- Do not merely paralyze the patient.
References
- Barry E, Hauser WA (1992)
Status epilepticus: the interaction of epilepsy and acute
brain disease. Neurology 43: 1473-1478. PubMed
- Hesdorffer DC, Logroscino
G, Cascino G, Annegers JF, Hauser WA (1998) Risk of
unprovoked seizure after acute symptomatic seizure: effect
of status epilepticus. Ann Neurol. 44: 908-12.
- Parent JM, Lowenstein DH
(1994) Treatment of refractory generalized status
epilepticus with continuous infusion of midazolam.
Neurology 44: 1837-1840. PubMed
- Ramsay RE, Hammond EJ,
Perchalski RJ, Wilder BJ (1979) Brain uptake of phenytoin,
phenobarbital, and diazepam. Arch Neurol. 36: 535-9.
PubMed
- Towne AR, Pellock JM, Ko D,
DeLorenzo RJ (1994) Determinants of mortality in status
epilepticus. Epilepsia 35: 27-34. PubMed
- Treiman DM, Meyers PD, Walton NY, Collins JF, Colling
C, Rowan AJ, Handforth A, Faught E, Calabrese VP, Uthman
BM, Ramsay RE, Mamdani MB (1998) A comparison of four
treatments for generalized convulsive status epilepticus.
Veterans Affairs Status Epilepticus Cooperative Study
Group. N Engl J Med. 339: 792-8.
- Treiman DM, Walton NY,
Kendrick C (1990) A progressive sequence of
electroencephalographic changes during generalized
convulsive status epilepticus. Epilepsy Res. 5: 49-60.
PubMed
- Wilder BJ (ed.) (1993) The use
of parenteral antiepileptic drugs & the role for
fosphenytoin. Neurology 46 suppl. 1. PubMed
- Working Group on Status
Epilepticus (1993) Treatment of status epilepticus:
recommendations of the Epilepsy Foundation of America's
Working Group on Status Epilepticus. JAMA 270:
854-859. PubMed
Last revised 07/25/2003
M. Steven Evans [ mail | epilepsy page ]